February 2, 2024 -View an updated version of this article.
February 2, 2023
Premera Blue Cross HMO, a subsidiary of Premera, recently launched the HMO Core Plus plan to employers in Pierce, Thurston, and Spokane counties. To ensure participating providers in the Sherwood HMO network are prepared to support HMO members, we have
provided responses to commonly asked questions.
Referrals
| Question: |
Answer: |
- If a patient sees a specialist without a referral from their PCP, who is responsible for payment, the patient or provider?
|
If there isn’t a referral, the service isn’t covered and the member is responsible for 100% of the cost for the services. Any amount won’t apply to their out-of-pocket maximum, except services required by federal or state law. |
- Can a provider (all areas of specialty) send in a referral after the patient sees the specialist?
|
Yes, a provider can send a post-service referral within 60 days of the date of service. |
- Can a specialist refer a patient to another specialist without getting authorization from the member’s assigned PCP?
|
Yes, an in-network specialist with an approved referral on file may submit a “secondary” referral to another in-network specialist without getting authorization from the member’s PCP. However, we encourage the referring specialist to consult
with the member’s PCP to ensure coordination of care. |
- Is it the responsibility of the referring provider to send the referral or for the specialist to request it?
|
It is the responsibility of the referring provider (member’s PCP or in-network specialist with an approved referral on file) to submit a request to a specialist. |
- If the specialist is not in-network and the out-of-network referral isn’t approved by Premera, does the member still have coverage?
|
No, there are no out-of-network benefits available as part of the Premera HMO plans, except for urgent or emergency situations.
|
Prior Authorization
| Question: |
Answer: |
| How do I submit a prior authorization? |
Submit all prior authorizations for Premera HMO through Availity, Premera’s secure provider portal.
Note: The prior authorization medical policies used for Premera HMO are the same as Premera’s other commercial lines of business.
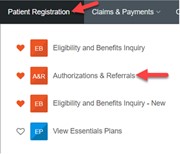
View Availity Quick Guide for online provider tools.
|
| What is Premera’s timeframe to complete a prior authorization or referral? |
We typically respond to requests within 1—2 days, but it can take up to 5 days. Check the Availity Auth/Referral dashboard for
status after submitting the authorization request. Note: Most requests will be auto approved if both the requesting and servicing provider are Sherwood HMO network providers. |
| Who is responsible for obtaining a prior authorization for a service: The referring PCP or the specialist performing the service? |
The specialist that is performing the service is responsible for obtaining a prior authorization when applicable. |
| Is authorization required for outpatient physical therapy? |
For SEBB (School Employees Benefits Board) HMO members, no authorization will be required for outpatient physical therapy.
For large group HMO members, outpatient physical, occupational, and massage therapy services are subject to medical necessity review for services beyond the
initial evaluation and subsequent 6 therapeutic visits, based on episode of care. Authorizations will need to be generated by the servicing provider through eviCore Healthcare. Sign in to eviCore Healthcare by logging onto www.evicore.com,
call 800-792-8751, or sending an eviCore Healthcare request form via fax to 800-540-2406.
|
Direct Access and Requirements for Specialists
Pharmacy
| Question: |
Answer: |
| Is there any difference in pharmacy services or drug coverage for HMO vs a non-HMO Premera plans? |
Most Premera HMO plans (SEBB not included) require the use of exclusive home delivery using the Express Scripts mail-order pharmacy for maintenance medications, designed to be a cost saving strategy for members.
The HMO Core Plus plan is a 4-tier plan using the Essentials formulary. It considers a drug’s clinical efficacy, safety, alternatives, and cost effectiveness in determining a drug tier. The purpose is to help direct members and providers
to the highest value medication options (quality/cost) when determining a patient care plan.
See Covered Drugs | Premera Blue Cross and select the E4-HMO drug list to learn more and access the full list of generic, brand and specialty drugs covered under this plan.
|
ID Card
| Question: |
Answer: |
| Will patients have a new ID number and/or a new ID card for the Premera Blue Cross HMO Core Plus plan? |
For our SEBB HMO members that are currently enrolled on a Premera plan in 2022, they will keep their current ID number and receive a new HMO-branded ID card.
For our large group HMO members that are currently enrolled on a Premera plan in 2022, they will receive a new ID number and ID card for the HMO plan.
|
Member Benefits and Eligibility
| Question: |
Answer: |
| Where can I find eligibility and benefit information for the Premera Blue Cross HMO Core Plus plan? |
Eligibility and benefits for Premera HMO are done through Availity, Premera’s secure provider portal. View Availity Quick Guide for online provider tools.
|
Looking for more information on HMO? Here are places you can get more information: