March 3, 2022
Eligibility and Benefits
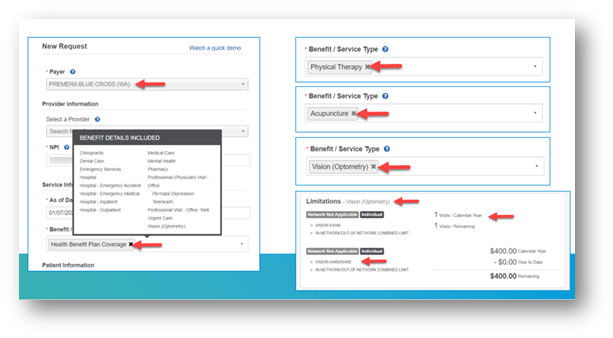
Through the Availity Eligibility and Benefits feature, you can check for general benefit information by selecting Health Benefit Plan Coverage from the Benefit/Service Type field. The hover-over feature shows you benefit details. This feature can help
you determine if you need to select a more specific benefit/service type (see sample screenshot showing physical therapy, acupuncture, or vision).
You can also use Health Benefit Plan Coverage to see if your patient has active vision coverage. For details, select Vision (Optometry) from the drop-down menu. This example shows the member has a $400 annual limit for vision hardware and $400 remaining
for the year.
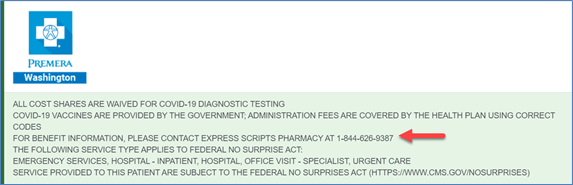
For member-specific plan information, check green box at the top of the Eligibility and Benefits page. Keep in mind this information can change and is specific to the member’s benefit plan and service type. Here’s an example:
Claim status
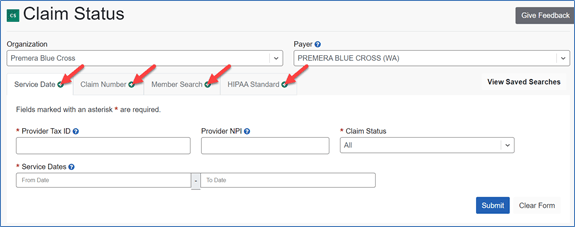
Use the Claim Status feature to check for a claim by service date, claim number, and member search (new feature added in February). The HIPAA Standard transaction tab is a standard option for all payers through Availity.
Using the enhanced Service Date tab, you only need to select your TIN for your provider organization and the dates of the service you’re looking for. To narrow the claims list, enter the provider’s NPI. You can then view a list of claims based on the
dates provided (2 years of claims data available) and details about each claim.
You can also link directly from the claim details page to Remittance Viewer to see more payment information about the claim and get a copy of your EOP.
Explanation of Payments
To find out more about how explanation of payments (EOPs) work in Availity, read our December
2021 Provider News article.
Prior authorization
You’ll still need to submit a prior authorization through Premera.com. Use the link in Premera’s payer space to see if a code requires a prior authorization, submit a prior authorization, or check the status of your requests. The Availity prior authorization
feature for Premera plans is scheduled to go live in second quarter 2022.
For more information
Visit
availity.com/Premera for helpful user guides, training, and other resources.
Remember that transactions for all our Individual Plans and Premera Medicare Advantage plan
members are not available through Availity. Check out recent provider workshop recordings linked in our Learning Center.