May 5, 2022
Providers seeing Premera Blue Cross members will soon have access to a new online prior authorizations experience on Availity Essentials. This new tool will be available by the end of second quarter.
Using Availity to submit your prior authorizations eliminates the need to fax your requests. Availity's prior authorization tool simplifies the submission process and enables a more user-friendly workflow.
Highlights include:
- Inpatient and Outpatient Prior Authorizations
Complete and submit inpatient and outpatient prior authorizations and get real-time responses for your Premera members.
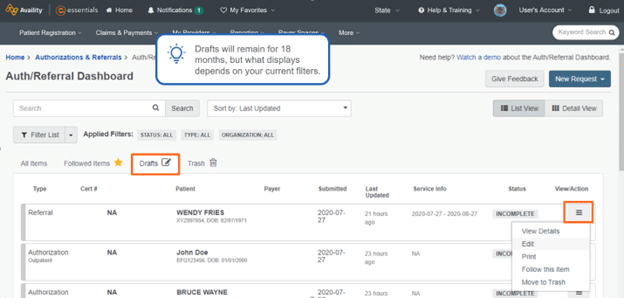
- Auth/Referral Dashboard
View all submitted prior authorization requests and statuses from a single page and use filtering options for easy prioritization.
- Auth/Referral Inquiry
Providers (service provider or facility) included on a request can check the status of a prior authorization request.
- Premera Code Check
Enter your procedure code to see if it requires a prior authorization.
- Attachments
An attachments feature allows you to add documentation to your initial request. (A maximum of 10 files allowed. Each file is limited to 10 MB or a combined total size of 50 MB.)
- Drafts
If you don't complete your request, it automatically saves as a draft in your dashboard for 18 months. To return to where you left off, select the "Drafts" tab where the status filter displays "Incomplete."