September 1, 2022
Premera is already live on Availity and we’re just six business days away from fully transitioning our secure online provider tools to Availity. Access to our secure tools on premera.com will no longer be available as of September 10, 2022.
3 Tips for Transition Success
- If you're already registered with Availity, you’re good to go. Use your existing user ID and password to work with Premera. If you’re a dental provider, choose Premera Dental as the payer.
- Register and get training or sign into Availity. Sign
up as soon as you can as it may take 2-3 days for your registration to process.
- Watch recorded training webinars that are specific to Premera. Simply sign in to Availity, select Help & Training > Get Trained.
Type "Premera" in the search catalog field and select the course you want.
Tools in Availity
Sign in to Availity to use the following tools:
| Eligibility and Benefits |
Use Member Search to search by a member’s plan ID number, first name, last name, or date of birth. |
| Claims and Payments |
Search claim status by claim number, member ID, or date range. Up to two years of claims and EOP data are available. |
| Prior Authorizations |
Complete and submit inpatient and outpatient authorizations and get real-time responses for your Premera members. Incomplete requests are automatically saved as drafts in your dashboard for 18 months. Note: Need to check
a code to see if an authorization is needed? Access Premera’s code check tool through Availity. The tool is available on the Authorizations & Referrals page under the Additional Authorizations and Referrals section. |
| Remittance Viewer/EOPs |
Review explanation of payments (EOPs) in the Check/EFT tab. Select the EOP icon under the Actions menu to download a PDF. Note: Use “Other Blue Plans” as a payer to view FEP check information. |
| Electronic Funds Transfer (EFT) |
Use EFT for enrollment or cancellation requests. (If you’re already signed up for EFT through Premera, no changes are required.) |
Note: Claims editor, PCP roster, and payment policies will remain on Premera’s secure provider website, but can also be found on the Premera payer space in Availity under Resources.
Reminders
Electronic Funds Transfer Enrollment Information for Premera Providers
If you’re already enrolled in Electronic Funds Transfer (EFT), you don’t need to re-enroll through Availity. Premera will still process Availity transactions for EFT requests. However, if you're a new provider, you must enroll for EFT using Availity’s Transaction Enrollment Tool. Watch this how-to demo or view an EFT enrollment help topic.
Call Availity for Technical Support
For Availity technical support or registration information, call 800-282-4548, 8 a.m. to 5 p.m., Eastern Time, Monday through Friday. To open a support ticket, sign in to your Availity account, select Help & Training, and then Availity Support in the upper-right area of the page.
New! Enter 5 Days Prior to Date of Service for Premera Inpatient Authorizations
Premera providers can now enter a date up to five days prior to the date of service in the "From Date" field on inpatient authorizations. Try it on your next inpatient authorization request. Learn more.
Plans Not Served Through Availity
Individual Plans and Medicare Advantage are not served through Availity. Availity’s Authorization & Referrals tool does not apply to Individual plans, Medicare Advantage, FEP, and Shared Admin. Prior authorization service requests that go through eviCore and AIM today will continue as is.
How to Check EOPs
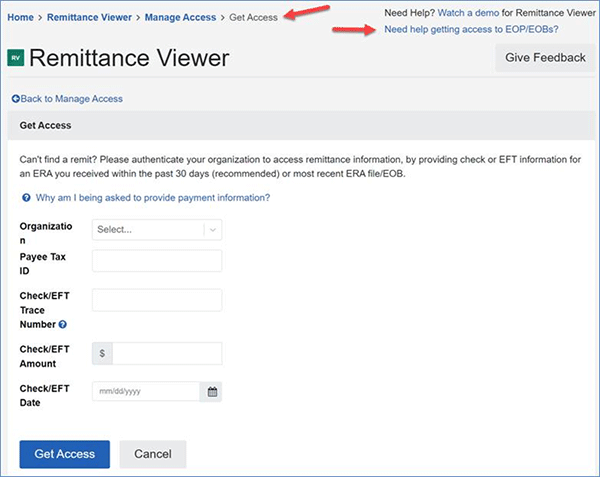
To see your check and explanation of payment (EOP) information that Premera submits to Availity, you’ll first need to validate a check from Premera. The check must be dated within the last 30 days. Then you’ll be able to see the check information and EOPs for Premera business. Check information and EOPs for the Federal Employee Program (FEP) are available when you select the payer option, “Other Blue Plans Premera BlueExchange (FEP, Shared Admin).” Information for Individual and Medicare Advantage plans is not available through Availity.
EOPs that were unavailable August 12-25 due to a brief processing delay are now available. We apologize for the inconvenience. View how to find your EOPs. Here's a sample Availity Remittance Viewer landing page:
More information
Availity provider FAQ
Quick Guide for registered Premera providers
Crosswalk for Availity vs. Premera secure tools (Availity sign-in required)