February 3, 2022
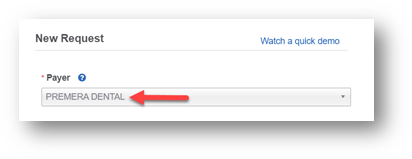
When using Availity to check dental benefits, remember to choose “Premera Dental” as the payer:
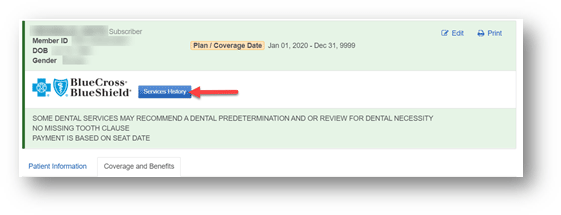
You can find a patient’s dental claim history by clicking on the blue Services History button at the top of the member’s eligibility and benefits page. This button displays only when you select Premera Dental as a payer.
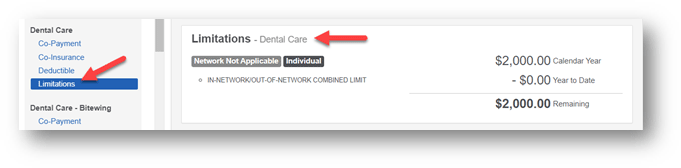
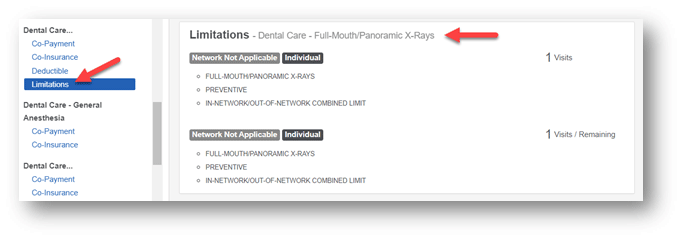
Verify benefit limits
If you’re looking for a member’s dental services benefit limits, you can:
- Scroll through the list of benefits to find the specific service limitations
- Use control F to open a search box and use the keyword ‘limit’ to view all dental services that have limitations.
Fee schedules for out-of-area dental providers
If you need a dental fee schedule, contact United Concordia.
For more information
For more Premera dental provider information, visit our Dental Resources page.