February 20, 2020
Our prior auth tool helps you check codes, confirm if a review is needed, get a reference number for your patient’s file, and more.
Our prior auth tool offers:
- Detailed requirements based on the patient’s diagnosis and benefit coverage
- Options for inpatient, infusion, and durable medical equipment (DME)
- Quick links to medical policies
- The ability to print a confirmation, attach documentation, and check status
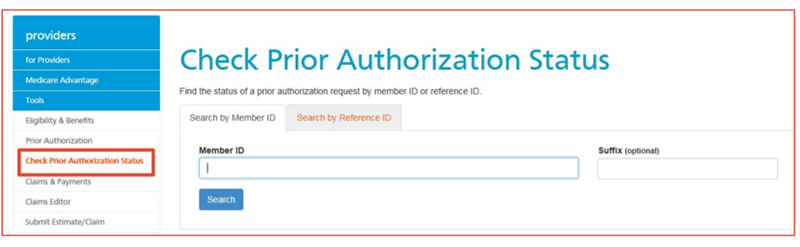
Checking prior auth request status
In some cases, you’ll receive immediate auto approval within the tool. You can also check status using the member or reference ID number, even if you didn’t submit the request online. (Note: Faxed requests can take up to 2 days to appear within the tool.) Keep in mind that we typically respond to your request within 5 calendar days. It may take up to 15 days if we need additional information.
For more information
To learn more, check out our step-by-step prior auth tool user guide for helpful tips and screenshots.