December 5, 2019
In 2020, a new outpatient facility edit will be implemented to check interim hospital claims with bill types ending in 2 or 3 against the discharge status code. If discharge status code 30 is not present on interim claims with frequency 2 or 3, the claim will be denied as inappropriate billing per UB-04 billing guidelines.
An interim claim is billed when a patient receives a continuous course of treatment in an outpatient department of a hospital which is expected to cover multiple months of care. These interim claims need to be coded correctly to identify the claim is part of ongoing care and the patient will continue to receive additional care.
Bills for a continuous course of treatment must be submitted in the same sequence in which the services were rendered. This results in interim claims being submitted for each month’s worth of services. If the interim claim is submitted out of sequence from the prior interim claim, it will be denied reimbursement.
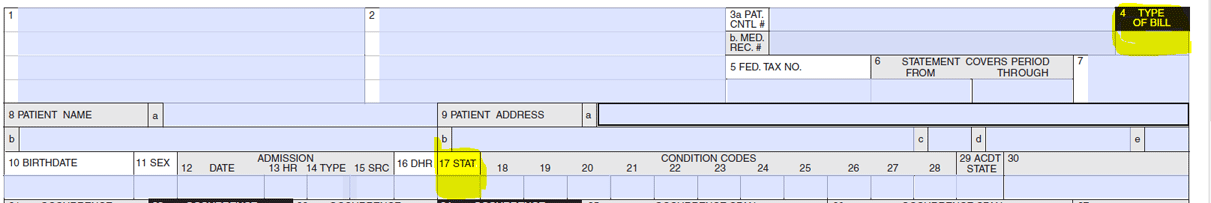
Interim claims are identified by the bill type code billed in field 4 on a UB-04 claim form (see field). The fourth digit in the Bill Type code identifies the frequency as follows:
- NNN2 – Interim - First Claim
- NNN3 – Interim – Continuing Claim
- NNN4 – Interim – Last Claim
The from and through dates on the claim (Field 6) indicate the date span covered by each Interim claim.
In addition, to indicate that the patient is still receiving care, a correct patient discharge status code is required on the claim as well. For any Interim claim with a bill type code that ends in frequency code 2 or 3, the required discharge code needed in field 17 is 30 – Still a Patient.
Once the final claim is submitted with bill type frequency code 4, the discharge code in field 17 should represent the final status of the patient such as discharged to home.