November 6, 2023
Your feedback helps us make meaningful changes within Availity as quickly as possible. Here are some helpful reminders, thanks to questions we’re hearing from providers.
If you have new office staff who need Availity training, they can view Premera’s Availity Tips and Resources video tutorial or check out our user guide.
Availity also offers Premera-specific webinars in the Availity Learning Center. Simply sign in to Availity, and go to the Availity Learning Center > Help &
Training > Get Trained and enter the keyword "Premera."
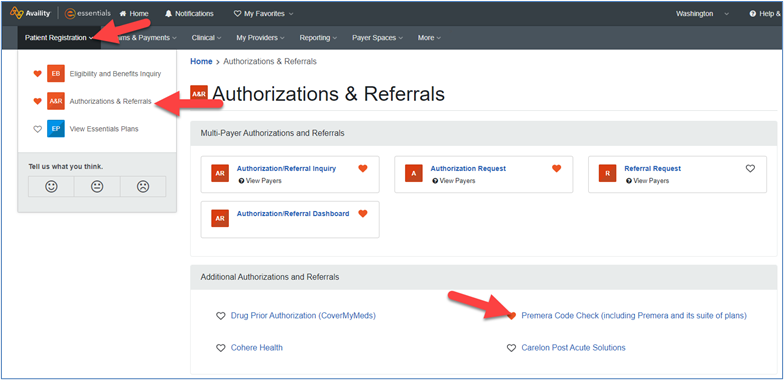
Which services typically need prior auth/overall prior auth info?
To do a quick general search to see if prior authorization is required for a service, use the Premera code check tool. Note that the code check tool isn't a guarantee of coverage since member contracts may differ in benefits.
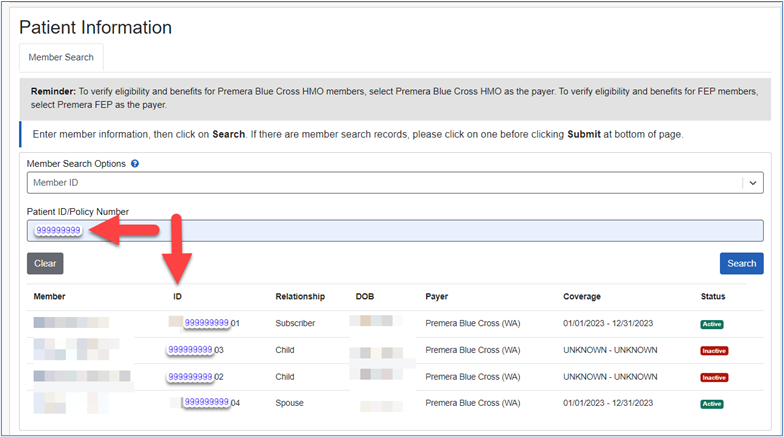
How can I find all members related to a single member ID?
When doing an eligibility and benefit search in Availity using Premera as the payer, only enter the 9-digit member ID in the “Patient ID/Policy Number” field. The results will display all the members attached to that member ID and the full member ID (includes
prefix, member ID, and suffix). Searches by Member ID will only display for Premera members.
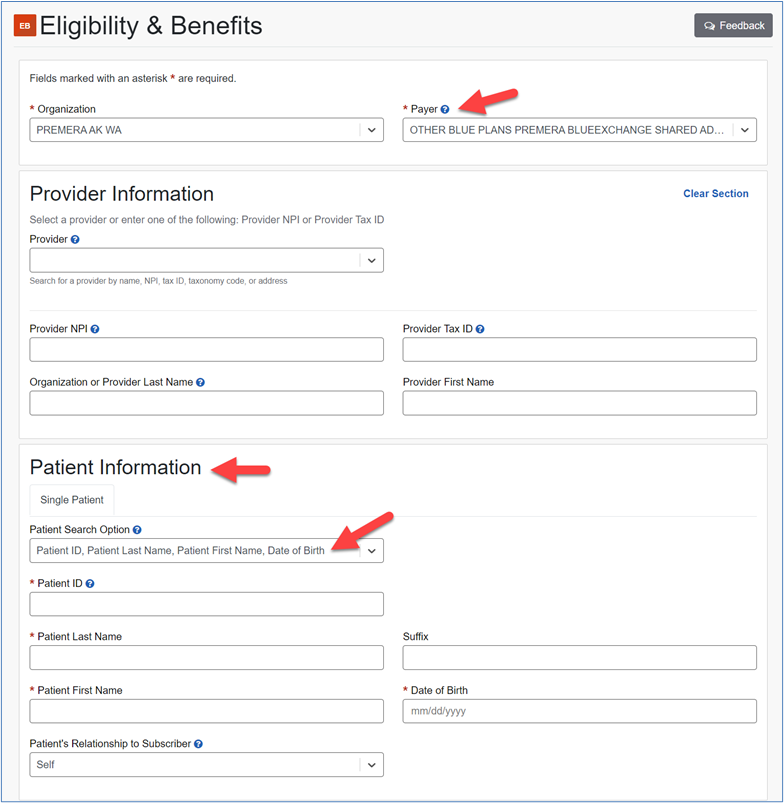
Note: For BlueCard and Shared Administration member eligibility and benefit searches, use “Other Blue Plans Premera BlueExchange Shared
Admin” as the payer and enter all the information for the member. This information is required to direct the request to the correct Blue plan for a response.
Can I do a BlueCard member eligibility and benefit search by member ID using Premera as the payer?
If you use Premera as the payer for a BlueCard member eligibility and benefit member ID search, the response will come back stating no member found. For BlueCard and Shared Administration member eligibility and benefit searches, use “Other Blue Plans
Premera BlueExchange Shared Admin” as the payer and enter all the information for the member (including member prefix, ID, and suffix). This information is required to direct the request to the correct Blue plan for a response.
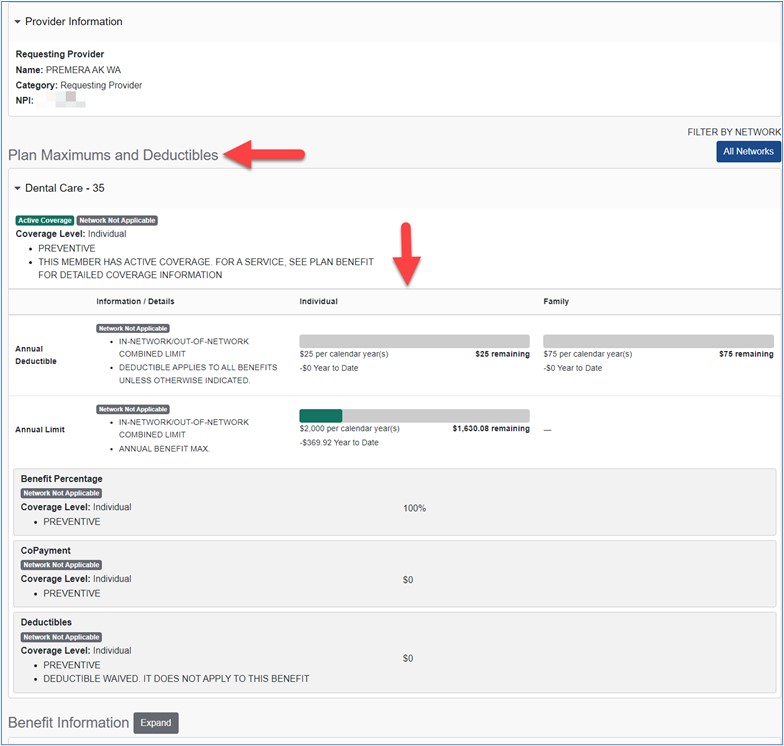
Dental enhancement added
Providers will now see the deductible and limits at the top of the eligibility and benefits results when using “Premera Dental” as the payer.
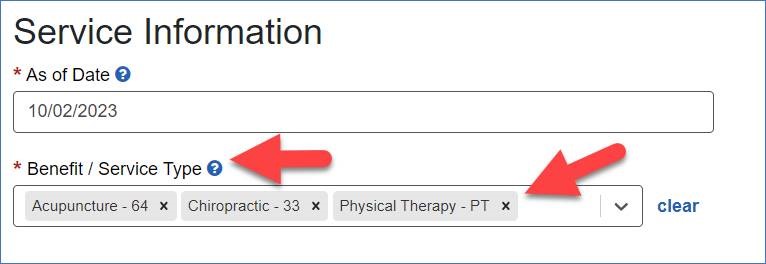
Where is the benefit information for acupuncture, chiropractic, or physical therapy?
To view information about a specific benefit, select “Acupuncture,” “Chiropractic,” or “Physical Therapy” under the Benefit/ Service Type when running an Eligibility & Benefit transaction.
Note: If there isn't a limit listed, then there is no yearly limit. However, note that medical necessity and billing guidelines still apply.