April 6, 2023
We’re listening to your feedback and making meaningful changes within Availity as quickly as possible. We receive feedback through customer service calls, provider support teams, and Availity's online feedback feature.
Here are some recent improvements we’ve made, based on what we’re hearing from providers:
| Provider Feedback: |
Solution: |
| "I can’t find benefit limits for physical therapy." |
Select "Physical Therapy" under the Benefit/ Service Type when running an Eligibility & Benefit transaction. If there isn't a limit listed, then there is no yearly limit. However, note that medical necessity and billing guidelines still apply. |
| "How do I figure out the frequency for specific dental codes?" |
Use the Ctrl + F keys and do a keyword search by the description (rather than a specific code) to find the frequency for a specific benefit or service. |
| "I need to verify if codes need prior authorization." |
In the top-right corner in Availity in the “Keyword Search” field, type "Code Check Tool.” You can use our code check tool to confirm if codes need prior authorization. The link to the tool is also located under Patient Registration> Authorizations
& Referrals> Additional Authorizations and Referrals section. Use the “♥” feature to save the tool to your favorites.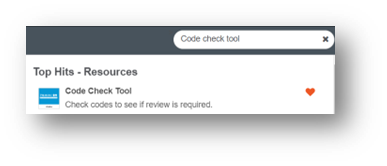 |
| "Can I submit an Amazon referral without calling?" |
In the top-right corner in Availity in the “Keyword Search” field, type "Amazon" to display a link to the Amazon In-Network Only Plan PCP Referral to Specialist form.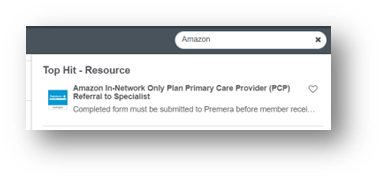 |
| "I’m required to call Premera and request a call reference number." |
Availity has transaction IDs which are the same as Premera call reference numbers. You can also print out the information with the date for your records. |
| Where do I find allergy benefits? |
We added a new benefit category called “Allergy Testing.” Information about Allergy Testing and Treatment, and Injections Therapeutic Allergy related services are all located under this new benefit category.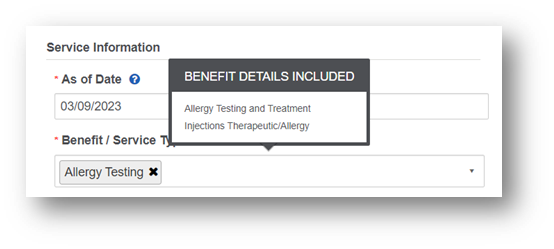 |
| How do I add Premera WA as a payer to my provider organization? |
If you need a state added to your provider organization’s account, have your Availity Administrator contact Availity Client Services at 800-282-4548, 8 a.m. to 8 p.m. ET, Monday through Friday. You can also contact them online by selecting
Help & Training > Availity Support. |