April 19, 2018
Thanks to great provider feedback, we've made even more improvements to our prior authorization tool.
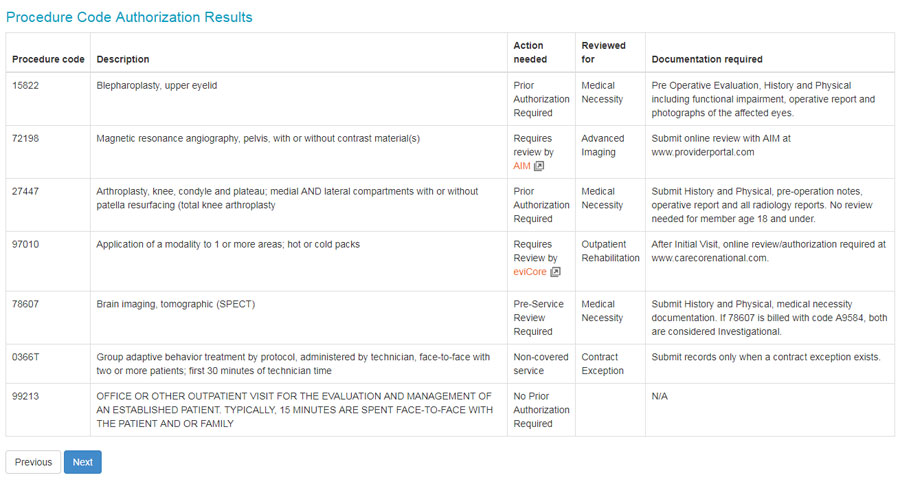
When you view results for procedures needing review, we’ll tell you when review is required and give you additional information that’s all in one place, including:
- What we’ll review the service for, such as medical necessity, contract exception, investigative, and more.
- Documentation requirements—highlighting the information you need to submit with your review request. This field will also tell you if there are age requirements for a service.
The screenshot below shows two new columns on the right for the procedure code review screen:
Providing this information makes it simpler for you to complete prior authorizations and pre-service reviews. It’s just one more way we’re making healthcare work better.
Check out our Prior Authorization Tool Guide for more information.