September 17, 2020
In July, the National Committee for Quality Assurance (NCQA) released proposed HEDIS® measure specification changes for the 2020 measurement year. NCQA will release final edits to specifications on October 1. Although edits to the specifications are possible, fundamental changes aren’t expected. Therefore, we’re providing advanced communication of important specification changes.
Key Updates
Controlling High Blood Pressure (CBP)
- This measure has a new definition: Hypertensive patients ages 18–85 whose blood pressure (BP) is adequately controlled (<140/90) during the measurement year. The last BP reading of the year determines compliance.
- Important changes:
- Patients are now identified for the measure by two outpatient visits with a diagnosis of hypertension between January 1 of the prior year and June 30 of the measure year.
- BP readings:
- BPs taken by a patient from any digital device are acceptable as long as the BP is documented in the patient’s legal record by the provider managing the patient’s BP.
- BP readings taken by the patient using a non-digital device, such as a manual blood pressure cuff and a stethoscope, are not allowed for HEDIS reporting.
- Patient self-reported blood pressure readings may be obtained during telehealth, telephone, e-visits and virtual check-ins.
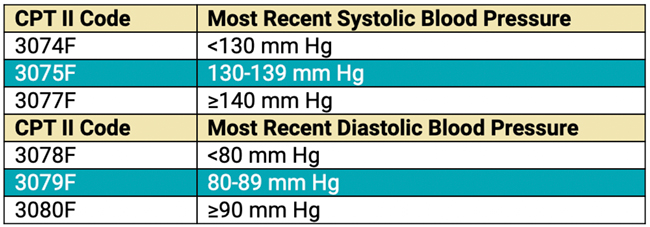
- Submit claims with BP CPT® II code results even if the BP isn’t compliant. Including CPT II result codes on the claim alleviates the need for a medical record request.
Palliative Care Exclusion
- Patients receiving palliative care are now excluded from the following measures:
- Breast Cancer Screening (BCS)
- Colorectal Cancer Screening (COL)
- Controlling High Blood Pressure (CBP)
- Comprehensive Diabetes Care (CDC)
- Statin Therapy for Patients with Cardiovascular Disease (SPC)
- Osteoporosis Management in Women who had a Fracture (OMW)
Advanced Illness Exclusion
- The following measures now allow advanced illness to be captured via telephone and e-visits:
- Breast Cancer Screening (BCS)
- Disease-Modifying Anti-Rheumatic Drug Therapy for Rheumatoid Arthritis (ART)
- Colorectal Cancer Screening (COL)
- Controlling High Blood Pressure (CBP)
- Comprehensive Diabetes Care (CDC)
- Statin Therapy for Patients with Cardiovascular Disease (SPC
- Osteoporosis Management in Women Who had a Fracture (OMW)
- Telephone and e-visit claims with advanced illness diagnoses will exclude patients from the measure if all exclusion requirements are met:
- 66 and older (67 and older for OMW)
- 2 advanced illness claims in the measurement year or the prior measurement year and a frailty code in the measurement year
- Frailty codes are required for the advanced illness exclusion but cannot be obtained through telephone or e-visit claim.
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA).
CPT Copyright 1995-2020 American Medical Association. All rights reserved. CPT® is a registered trademark of the American Medical Association.