August 18, 2022
Healthcare quality and cost can greatly vary between one provider and another. This contributes to what we refer to as the four problems of healthcare:
- With too much variation, members experience care that costs too much instead of cost-efficient care.
- They’re not getting what they need when they should be receiving effective care.
- They’re even getting what they don’t need instead of receiving appropriate care.
- And they aren’t having the experience they feel they deserve when they should have an exceptional experience.
How do we address this?
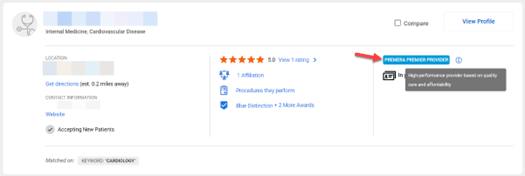
To help members navigate and recognize high-performing providers, the Premera Premier Provider program designates providers as either high quality, cost efficient, or both. These high-performance designations are featured on member-facing provider search tools and used by Premera in its service model to customers. If a provider is designated, the appropriate designation (high performance, quality, and/or cost efficiency) will display in the provider information available to Premera members (see snapshot below).
What updates are we making to improve the program?
Beginning August 2022, the Premera Premier Provider designation program will:
- Expand to include physician assistant and nurse practitioner performance
- Extend the review period to calendar years 2019, 2020, and 2021
- Include an updated, robust data set for inpatient and outpatient quality measurement
The Premera Premier Provider program will not impact customer rates. Members can continue to see their current provider(s), regardless of the provider’s designation status. If a provider is still in a member’s plan network, the in-network rate will not change.
The fact that a provider isn’t designated doesn’t mean they don’t provide quality and cost-effective care. In order to qualify for a designation, providers must have adequate data and must practice within one of the 12 assessed specialties. All in-network providers meet minimum quality standards laid out by the Blue Cross Blue Shield Association.
More about the Premier Provider Program
If you’re interested in more information about the Premera Premier Provider program, visit our webpage which includes a detailed program methodology white paper, the program summary, FAQs, and contact information.